Retina / Diabetic Retinopathy
What is diabetic retinopathy or diabetic eye disease?
Diabetic retinopathy or diabetic eye disease is a vascular disease caused by metabolic changes suffered by patients with diabetes, and it is the most common cause of blindness in Spain for those of a working age.
Diabetes can cause serious vision problems for the following reasons:
● Retina problems: 1 in 10 patients with diabetes in Spain suffer from some degree of diabetic retinopathy or macular atrophy. That is why it is essential to examine the back of the eye at least once a year, so this disease can be detected early. 1 in 50 diabetes patients in Spain suffers from diabetic macula edema.
● Cataracts: these develop earlier in patients with diabetes.
● Glaucoma: patients with diabetes have a higher risk of developing glaucoma.
Types of diabetic retinopathy
Non-proliferative diabetic retinopathy (NPDR)
Proliferative diabetic retinopathy
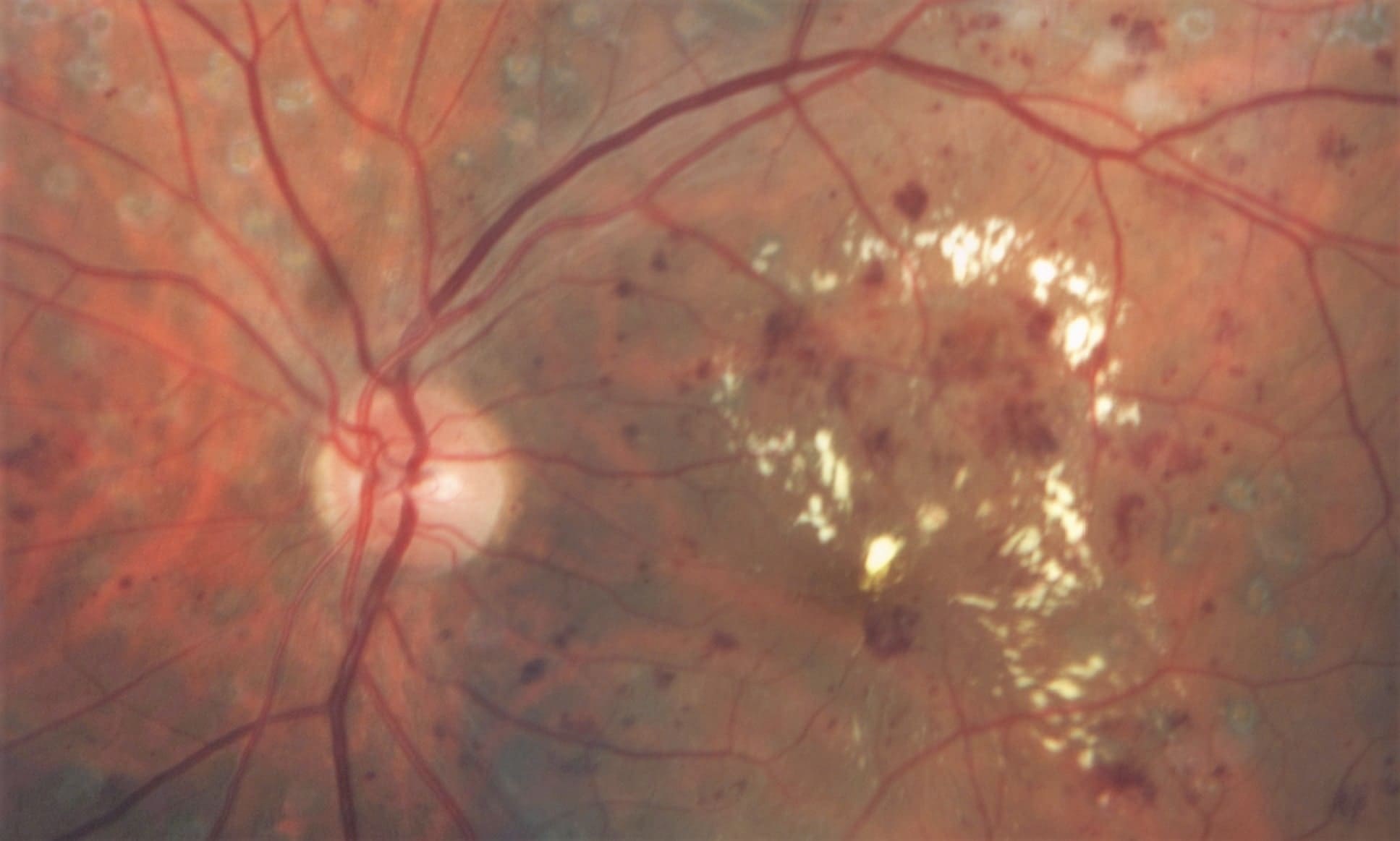
This is the earliest stage of diabetic retinopathy which involves the appearance of microaneurysms, where blood vessels break down and allow blood to leak into the eye.
Deposits of cholesterol or other fats from the blood can enter the retina, forming what looks like blisters.
As the disease progresses, this type of mild non-proliferative retinopathy can develop into a moderate form when some of the blood vessels supplying the retina get blocked, which will complicate the situation as the blood supply to the retina will be stopped.
Some of the consequences for the retina are haemorrhages within the retina itself and inflammation or thickening of the macula due to fluid leaking from blood vessels in the retina (hard exudates), with macular oedema and retinal venous occlusion being the most common cause of vision loss in patients with diabetes.
Macular ischaemia may also occur, where the blood vessels close or become clogged and vision becomes blurred because the macula does not receive enough blood.
This advanced stage of retinopathy may lead to central and peripheral loss of vision. This occurs when blood vessels in the retina become clogged and prevent sufficient blood flow, and new, thinner and more fragile blood vessels develop in an attempt to supply the retina with blood. This process is called neovascularisation.
These vessels develop throughout the retina and the surface of the vitreous gel. They do not cause any symptoms or loss of vision, but if they leak blood, they could lead to severe loss of vision, or even blindness. If the new vessels are also accompanied by scar tissue, they could cause the retina to wrinkle or detach.
Some of the consequences of this are as follows:
→ Vitreous haemorrhages: where the new blood vessels bleed into the vitreous. A vitreous haemorrhage alone will not lead to loss of vision.
→ Retinal detachment due to traction: this happens when the retina becomes wrinkled and possibly becomes detached. The loss of vision will be very serious if the macula or larger areas of the retina become detached. When the blood is removed, the patient’s vision may return to normal, if the macula has not been damaged.
→ Neovascular glaucoma: the pressure on the eye increases, which causes a particularly serious condition to develop that causes damage to the optic nerve. Once the blood is removed, the patient’s vision may return to normal, provided that the macula has not been damaged.
Causes of diabetic retinopathy
Diabetes mellitus (DM) causes abnormal changes to sugar levels in blood (glucose) that is converted into energy to power all the body’s functions. If diabetes is not managed correctly, the high levels of sugar in the blood will build up in the blood vessels, blocking blood flow to the body’s organs, including the eyes.
Diabetes is generally classified into two different types:
With both types of diabetes, abnormal spikes in blood sugar levels can increase the risk of diabetic retinopathy. The eyes can become damaged when these high sugar levels in the blood become chronic and begin damaging the blood vessels in the retina.
→ Type 1 diabetes: when the patient is deemed to be dependent on insulin, as they need injections or other medication to supply the insulin that their body is not capable of producing by itself. Insulin is a natural hormone that helps to regulate the sugar levels in the blood that are necessary for providing the body with energy.
→ Type 2 diabetes: when the patient is not considered dependent on insulin, or is insulin resistant. In this case, the patient produces enough insulin themselves, but their body cannot use it correctly. To compensate, their body will produce even more insulin than normal, which may lead to an abnormal increase in blood sugar level.
Symptoms of diabetic retinopathy
The main problem with this disorder is that there are no symptoms during the early stages or even the advanced stages. That is why early detection programmes are so important to avoid blindness in patients with diabetes.
Not even patients who manage their metabolism perfectly are exempt from potential complications.
All diabetes patients should have the back of their eyes examined on a regular basis, with the frequency depending on the condition of their eyes.
In advanced stages, symptoms include:
→ Difficulties with reading.
→ Blurry central vision.
→ Defects in central field of vision.
→ Floaters.
→ Sudden and complete loss of vision.
Diagnosing diabetic retinopathy
The signs that develop on the back of the eye are very specific and easy to identify for expert retinologists.
→ Dot haemorrhages or microaneurysms.
→ Soft exudates (cotton wool spots).
→ Macular edema.
→ Retinal haemorrhages that do not affect vision.
→ Hard (lipid) exudates.
To diagnose this disorder, the back of the eye should be examined with at least one central photograph of the retina, using OCT angiography, a very precise and detailed diagnostic test for detecting any retinal disease that may threaten your vision.
And, of course, this should also ideally be combined with a comprehensive examination using the following diagnostic tests:
Examination with dilation
This is a test where the pupils are dilated to examine the entire retina and the optic nerve, using eye drops to make the pupils larger.
Examination with slit lamp
This test enables us to view the different areas of the eyeball so we can examine it in detail, from the front to the back of the eye.
Visual acuity test
This enables us to measure the patient’s ability to see objects in detail from a certain distance.
Fluorescein angiography
This is used for examining the blood vessels in the retina.
Optical coherence tomography (OCT)
This is a diagnostic, control and monitoring test, that enables us to examine the retina in great detail. Optical Coherence Tomography (OCT) was a major advance in the study of the posterior pole of the eye (macula, retina and vitreous); it is very useful for diagnosing and surgically treating various retinal disorders.
Risk factors for diabetic retinopathy
1 in 5 diabetes patients develop this retinal disorder. It is important to bear in mind that this figure refers to all levels of the disorder. This means that we are not necessarily talking about the frequency of the disorder that threatens vision.
So, who has the highest chance of contracting diabetic retinopathy?
Blood sugar levels
High levels of glucose in the blood will increase the risk of diabetic retinopathy. As such, controlling blood sugar levels is key to preventing the appearance or progression of this disorder.
Blood pressure
High blood pressure is also a highly significant risk factor. The ideal blood pressure for the majority of people with diabetes should be less than 130/80 mmHg.
Duration of diabetes
The risk of developing diabetic retinopathy, or of it progressing, increases over time. As such, the probability of blindness is associated with the duration of the diabetes. For patients who have suffered with diabetes for over 30 years the probability can be up to 12%, whereas this drops to 7% in patients who have had the disease for 20 to 24 years.
Lipids in the blood
A high level of lipids in the blood may lead to a high build-up of exudates, the protein deposits that leak into the retina. This condition is associated with a higher risk of moderate visual loss.
Ethnic origin
Certain groups of people are more prone to developing diabetic retinopathy, primarily African Americans, Latinos and Native Americans.
Pregnancy
In pregnant patients with diabetic retinopathy, the disease will advance faster.
Treating diabetic retinopathy
Depending on the severity of the retinopathy, it may be treated with laser technology (photocoagulation), injection of antiangiogenic medication into the eye, or retinal surgery (vitrectomy).
The earlier diabetic retinopathy is diagnosed, the easier it will be to manage it effectively.
In other cases, when the retinal or macular disorder is very advanced, vitrectomy surgery may help to drastically improve the patient’s vision, and prevent or repair retinal detachment caused by diabetes.
→ Macular disorders caused by diabetes can now be treated very effectively with intraocular injections of various medications, which may also treat retinal disorders.
→ Retinal disorders caused by diabetes may require laser treatment to prevent progression of the disease and serious loss of vision.
Laser photocoagulation
La Laser photocoagulation is now a standard treatment for diabetic retinopathy and diabetic macular edema.
This procedure, which is performed using anaesthetic eye drops, involves applying a laser to the affected area. It should only take the specialist a few minutes to complete the surgery, but this will depend on the severity of the problem.
It may have a dazzling effect at first, due to the brightness of the laser beam. The patient’s eye should heal within two to six weeks, and it is normal for their vision to be worse at first, but it will come back once they have recovered.
If the retina has been damaged, this treatment will slow down progression of the disease as much as possible.
Vitrectomy
Vitrectomy is an effective procedure for treating loss of vision caused by diabetic retinopathy.
People with proliferative retinopathy have a less than five percent chance of going blind within five years after the surgery if they have received the right treatment early enough.
It is a procedure performed under local or general anaesthetic where the specialist will make a small incision in the eye to remove the vitreous gel that is clouded by blood, then replace it with a saline solution.
If the vitrectomy needs to be performed on both eyes, the surgery will be carried out on one eye at a time, with a week in between, so the patient can go home the same day.
Intravitreal injection
Intravitreal injections are used to locally administer medication to treat various kinds of secondary complications caused by diabetic retinopathy.
They are intended primarily for cases of diabetic macular edema (where there is excessive fluid in the macula). Corticoid or antiangiogenic medication is injected into the eyeball.
Treating diabetic retinopathy
The best treatment for diabetic retinopathy is prevention, which requires early detection. Properly managing blood glucose levels and blood pressure, following a healthy diet, doing exercise and educating diabetic patients on healthy lifestyles are essential factors to prevent or delay the appearance of diabetic retinopathy.
As such, although diabetes cannot be cured, we can prevent it from advancing further and we can ensure good quality vision as long as the condition is detected in time and managed properly. Therefore, the most important thing is for patients with diabetic eye disease to rigorously monitor their condition with regular visits to the ophthalmologist, and also follow a healthy diet as prescribed by a specialist endocrinologist.
Examinations of the back of the eye must also be adapted to the actual needs of patients, but as a general rule, a full ophthalmological examination should be performed as soon as the disease is diagnosed.
For sufferers of type 1 diabetes, the standard is 1 examination per year. On the other hand, patients with type 2 diabetes who manage the condition without medication could wait up to 5 years for each examination, given the low probability of developing retinopathy in the early stages of the disease.